Editor’s note: Discover the current COVID-19 news and assistance in Medscape’s Coronavirus Resource Center.
.
Clinicians have been combating COVID-19 wrong, says an emergency situation medicine doctor who has been on the front line of the COVID-19 surge in New york city City. “Everyone’s coming in too late.”
Richard Levitan, MD, invested 10 days in early April operating at Manhattan’s Bellevue Medical facility Center at the height of the COVID-19 surge.
” The x-rays I saw were all the very same: multi-lobar pneumonia,” he stated. “If we might identify it previously, we might initiate treatment earlier. We need to alter messaging to the general public, to physicians, to get earlier recognition of the illness.”
Levitan states that usage of house finger pulse oximeters by patients with COVID-19 might preempt the precipitous oxygen desaturation that causes a crisis that needs intensive care.
This would greatly lower the existing pressure on hospitals, he informed Medscape Medical News
Levitan argued in a current New York City Times viewpoint piece that everyone requires a pulse oximeter in their pandemic supply kit. The notion hit a nerve: more than 1500 remarks flowed in to the NYT site, and Levitan’s Twitter feed took off.
” I think earlier detection and treatment will make a huge distinction,” he stated.
But could such an easy, budget-friendly gadget as a finger pulse oximeter be the supreme weapon in this pandemic? Some specialists are not persuaded.
Levitan’s post “is definitely a remarkable theory, but I am unsure that pulse oximetry will be the trick to reducing COVID mortality,” David Hill, MD, a pulmonary and crucial care professional in Waterbury, Connecticut, and a representative for the American Lung Association (ALA), told Medscape Medical News
” Levitan’s supposition that clients who are hypoxemic are breathing more deeply and triggering their own lung injury is a leap,” he stated in an email. “Ventilators can cause lung injury by delivering greater pressures to the lung, but I am not familiar with any information recommending increased respiration in non-intubated patients with hypoxemia causes lung injury.”
Red Zone vs Blue Zone
.
Levitan, who is president of Air passage Webcam Technologies, a company that teaches courses in intubation and respiratory tract management in Littleton, New Hampshire, has invested 25 years in the field. He has actually produced a graphic highlighting how pulse oximetry could shift the battle lines to attack an earlier type of the illness with treatments like high-flow nasal cannula oxygen supplementation, constant favorable respiratory tract pressure (CPAP) devices, and client positioning/proning.
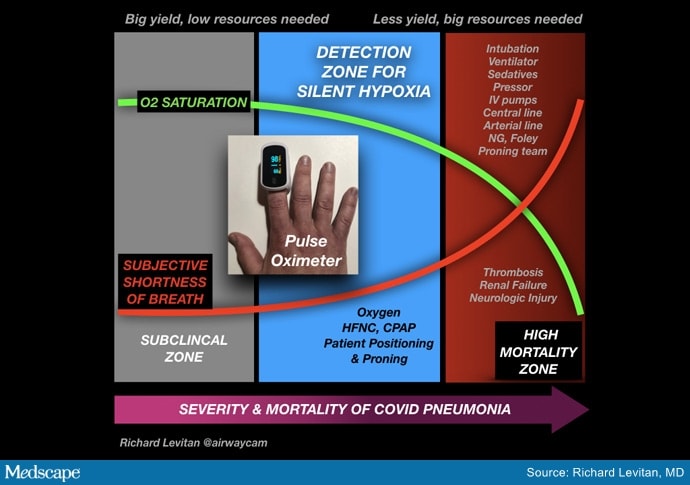
” If we move the whole window of treatment from the red zone into the blue zone, there will be a logarithmic collapse of the resources required to fight this illness.
” Clinicians require some way to win,” he added in an interview. “Waiting for individuals to have pulse ox saturations in the 50 s and 60 s is requesting for a tsunami of the walking dead.”
However “the strolling dead” phenomenon is indeed what ER physicians are presently reporting with numerous COVID-19 clients.
” These clients did not report any experience of breathing problems, although their chest x-rays showed diffuse pneumonia and their oxygen was listed below normal,” Levitan points out.
” I am seeing patients with oxygen saturations of 50%– approximately comparable to what you ‘d see at the top of Everest,” he informed Medscape Medical News. “It is amazing– shockingly fantastic– that these individuals are alive and talking on their mobile phone.”
Other physicians have likewise noted this and have recommended that some cases of COVID-19 pneumonia resemble high-altitude pulmonary edema (HAPE) instead of severe breathing distress syndrome (ARDS), but professionals in HAPE have pressed back on that tip.
Sooner Rather Than Later Always Better?
.
Erik R. Swenson, MD, a lung specialist and teacher of medicine at the University of Washington, Seattle, thinks using a pulse oximeter to find innovative pneumonia previously might be a great concept. He routinely encourages his clients to check their oximetry anyhow and concurs it ought to be recommended for clients with COVID-19
” There’s something about this infection that has people dropping their oxygen levels without the usual distress,” Swenson told Medscape Medical News. “It seems to cause you to lose that experience, the regular alarms aren’t going off, you’re not getting breathless or tachycardic.
” This is probably a sign the virus is injuring the lung,” he kept in mind. “Without treatments, we do not understand whether capturing this earlier is going to make any substantial distinction, however I believe basic principles would say that capturing anything sooner instead of later on is always much better, and we can constantly offer oxygen.”
The ALA’s Hill is more dubious about its utility.
Nevertheless, Hill added, “I would suspect that most of patients who weaken with COVID-19 are weakening due to progression of their viral disease and systemic inflammatory reaction rather than quiet hypoxemia causing them to increase their respiration and induce lung injury.”
Much about COVID-19 is still unknown, he said, and “unexpected deterioration in clients might be due to direct heart injury, increased thickening with heart, lung, or CNS effects rather than progressive quiet hypoxemia.”
However, Hill yields that “pulse oximeters are reasonably affordable (if readily available),” and supplying them to patients with thought COVID-19 for keeping an eye on “would likely have little downside.”
He kept in mind, though, that identifying moderate hypoxemia and tachycardia in clients who would otherwise do fine “might add to service provider workload and possibly ER visits.”
Patients would likewise require to be trained on appropriate use, ie, “no nail polish or synthetic nails, making sure their hands are warm when inspecting oximetry,” he added.
Another emergency physician, Jeremy Samuel Faust, MD, from Brigham and Women’s Hospital in Boston, who describes Levitan as “a terrific doc and a good friend,” states he also has some concerns about the general public’s response.
” While I think some pulse oximetry for patients with a known diagnosis of SARS-CoV-2 makes sense, I don’t support half the country buying these devices now on a ‘just in case’ basis,” he informed Medscape Medical News
Sales of pulse oximeters surged very early in the COVID-19 crisis, according to a report in Quartz, with a more than 500%increase already in mid-January.
In addition, Faust added that “as with any home medical devices, there’s constantly the issue of over-triage. There is undoubtedly such a thing as examining your numbers frequently. Transient and spurious readings can result in unneeded worry, and this can send out clients to clinics and emergency situation departments unnecessarily.”
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
.






