By Eric Ting, SFGATE
Published
-

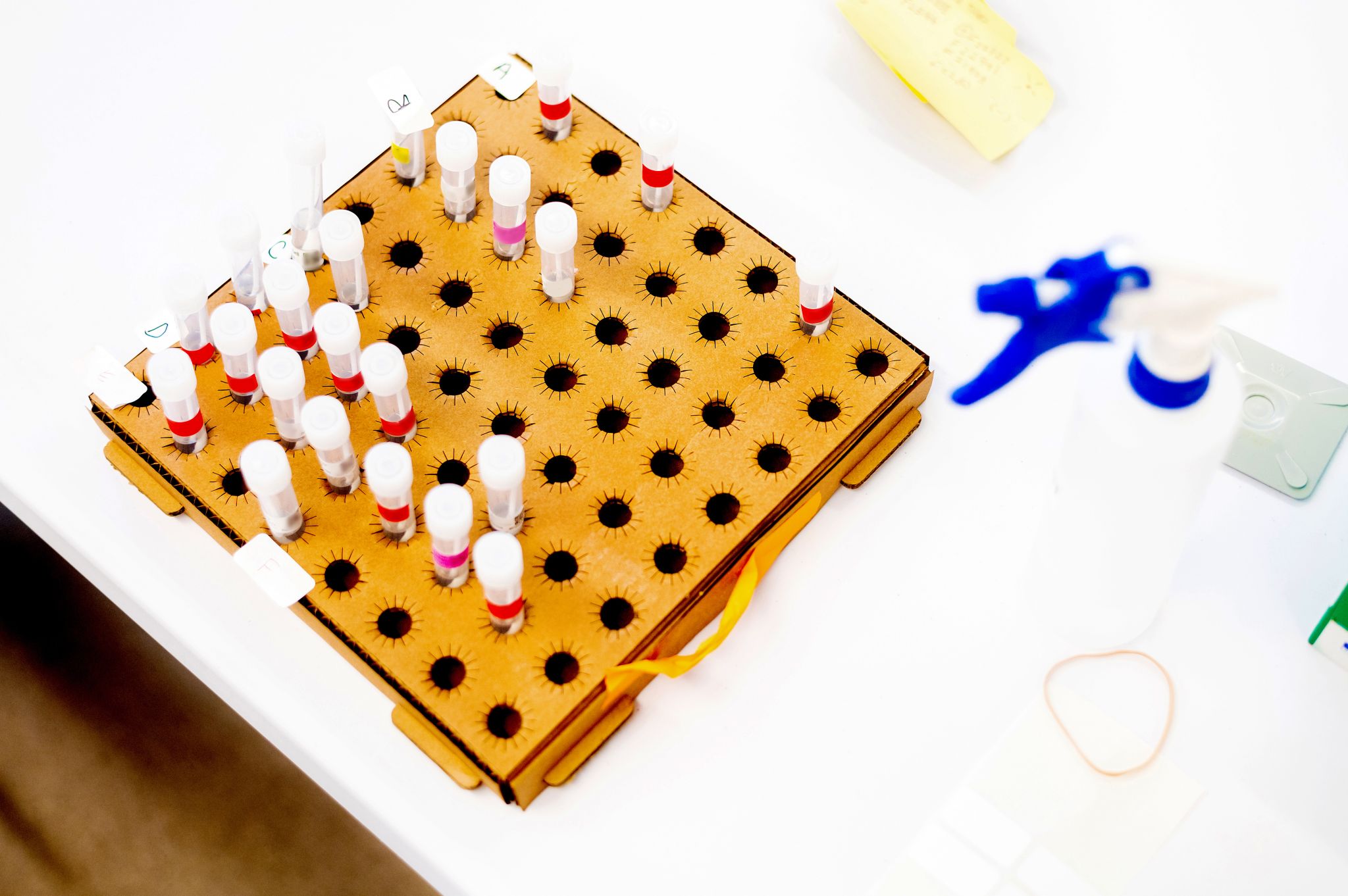
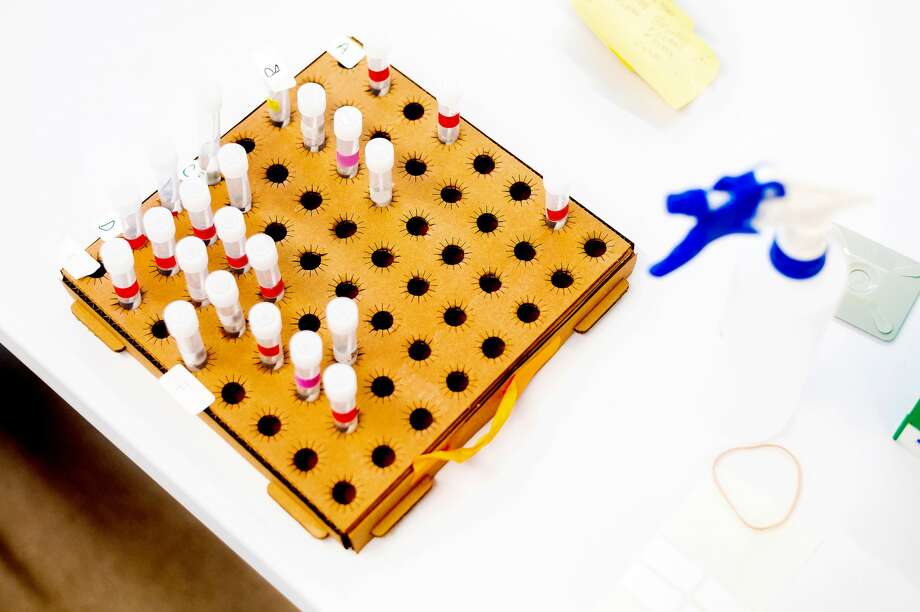
UCSF scientists process COVID-19 test samples at a new UCSF diagnostic laboratory adjacent to the Chan Zuckerberg Biohub (CZ Biohub) on Friday, April 24, 2020, in San Francisco.
UCSF scientists process COVID-19 test samples at a new UCSF diagnostic laboratory adjacent to the Chan Zuckerberg Biohub (CZ Biohub) on Friday, April 24, 2020, in San Francisco.
Photo: Noah Berger For UCSF
Photo: Noah Berger For UCSF
UCSF scientists process COVID-19 test samples at a new UCSF diagnostic laboratory adjacent to the Chan Zuckerberg Biohub (CZ Biohub) on Friday, April 24, 2020, in San Francisco.
UCSF scientists process COVID-19 test samples at a new UCSF diagnostic laboratory adjacent to the Chan Zuckerberg Biohub (CZ Biohub) on Friday, April 24, 2020, in San Francisco.
Photo: Noah Berger For UCSF
As both active virus and antibody testing ramps up across the country, it will soon be relatively easy for individuals to get tested, regardless of if one is displaying COVID-19 symptoms.
If you plan to get a test — either antibody or active virus — here is what you should know about the accuracy of the results.
Active virus testing (Diagnostic or PCR test)
The most widely available form of testing is PCR (polymearse chain reaction) testing, which detects if an individual is currently infected with the coronavirus.
Cleveland Clinic researchers tested 239 specimens known to contain the virus using some of the most commonly used coronavirus PCR tests. Here are the findings for each:
The CDC-developed test, which returns results in a few days, detected 100% of positive samples. A similar test from Roche detected 96.5% of samples, and a test from Cepheid that produces results in less than hour detected 98.2% of positive samples. However, Abbott’s ID NOW test — one that returns results in less than 15 minutes — detected virus in only 85.2% of positive samples, meaning it had a false negative rate of 14.8%.
Dr. Gary Procop, the head of the study, told NPR a test should be at least 95% reliable.
“So that means if you had 100 patients that were positive, 15% of those patients would be falsely called negative,” he said. “They’d be told that they’re negative for COVID when they’re really positive. That’s not too good.”
Abbott defended the test, and said potential problems could stem from storing samples in a solution called “viral transport media” before insertion into the testing machine. The company advocates for placing samples directly into the testing machine to ensure the most accurate results.
Generally speaking however, most PCR tests are considered to be very reliable.
Antibody testing
Considerably less reliable are antibody tests, which detect past infections by seeing if an individual’s immune system has developed protective antibodies.
The FDA has issued emergency approval for the production of several antibody tests, but the agency is now tightening regulations on approval given the unreliability of existing tests. Unlike PCR testing, where false negatives are what give scientists the most worry, antibody tests should strive to avoid false positives as it is more dangerous to tell an individual he or she has COVID-19 antibodies — and may have immunity — when that is not the case.
In a study of 14 of the approved tests, one of the tests gave false positives more than 15% of the time, and three others gave false positives more than 10% of the time.
“That’s terrible, said Dr. Caryn Bern, one of the study’s authors. “That’s really terrible.”
Three different tests had false positive rates of 1% or less, but all had false negative rates of over 10%, meaning they failed to detect antibodies in at least one of 10 actual infections. Observers concluded that none of the currently widely available antibody tests can be considered completely reliable as a result.
“Those numbers are just unacceptable,” Scott Hensley, a microbiologist at the University of Pennsylvania, told the New York Times. “The tone of the paper is, ‘Look how good the tests are.’ But I look at these data, and I don’t really see that.”
Earlier this week, a new antibody developed by Roche was approved by the FDA, and is considered to be the most accurate antibody test developed to date. Roche states the test detects antibodies with 100% accuracy, and has a false positive rate of just 0.2%.
MORE CORONAVIRUS COVERAGE:
Sign up for ‘The Daily’ newsletter for the latest on coronavirus here.
- California releases detailed list of outdoor activities allowed during shutdown
- SF’s COVID-19 case data by ZIP code reveals hardest-hit neighborhoods
- Should Bay Area swimming pools be allowed to reopen with other outdoor activities?
- San Mateo County to reopen 13 parks
- San Francisco finally closes JFK Drive in Golden Gate Park to traffic
- China study suggests outdoor transmission of COVID-19 may be rare
- Future of flying may include plastic shields, backwards seats and higher fares
- Trader Joe’s explains why the store won’t be starting curbside pickup or grocery delivery
- China study suggests outdoor transmission of COVID-19 may be rare
- Bay Area town to become one of 1st in world to test every resident
- U.S. restaurants will reopen with a different look. China gives clues as to how.
- ‘The weirdest thing is growing this bump by yourself’: What pregnancy and birth are like in a pandemic
- Study: Closing schools might not be worth the disruption
- Folsom Street Fair will be held online this year
- Will Portola Valley’s 168-year-old Alpine Inn make it to year 169?
- ‘Business has been incredible’: Inside one of the few SF businesses thriving during the pandemic
- New drone footage of shutdown SF eerily evokes film noir
- China study suggests outdoor transmission of COVID-19 may be rare
- Hayes Valley location of The Grove to close, Fillmore location could be next
- Boba Guys re-opens first SF location, half of former employees ‘not comfortable coming back’
Eric Ting is an SFGATE digital reporter. Email: eric.ting@sfgate.com | Twitter:@_ericting