An island community in Washington State has developed a testing and tracing strategy it hopes will be a model for rural and tribal communities.

In mid-March, Dr. Jim Bristow’s wife came down with gastrointestinal issues. Then, she couldn’t stop coughing.
Her symptoms pointed to coronavirus, but she couldn’t get tested — in part because of the nationwide test shortage, but also because the pair lived in Vashon, an idyllic town on an island in Washington State’s Puget Sound with scant medical resources. When Dr. Anthony S. Fauci of President Trump’s coronavirus task force said that the United States was failing with regards to testing, Dr. Bristow, said that it “really struck me.”
Dr. Bristow felt inspired to collaborate with other members in the Vashon community to develop a model to test, trace and isolate — in essence, a coronavirus response plan that they call the Rural Test & Trace Toolkit. Dr. Bristow, a retired cardiologist who was trained at the start of the AIDS epidemic, now believes that their model can be replicated, or serve as a guideline, for other isolated parts of the United States, including rural and tribal communities as they continue to face outbreaks.
As the novel coronavirus expands beyond major cities and the coasts — and as states start to emerge from shelter-in-place orders — locations with fewer medical resources will need strategies that work for them.
“While rural areas are typically underresourced and disadvantaged as it comes to health and health care, a model like this shows that rural places can be particularly nimble and flexible,” said Carrie Henning-Smith, the deputy director of the University of Minnesota’s Rural Health Research Center.
Image
Image
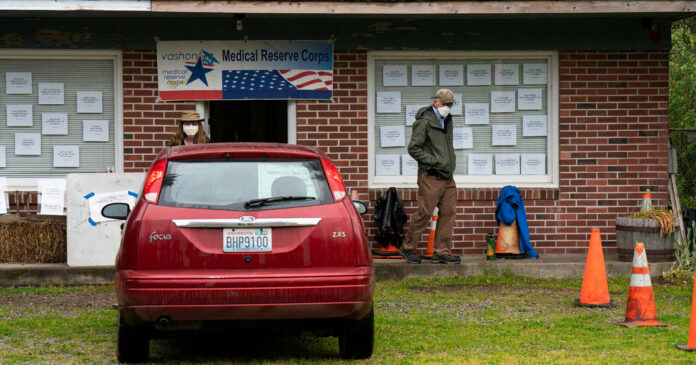
Although Vashon Island is geographically part of King County — which includes Seattle, the early epicenter of the coronavirus outbreak in the United States — it is unincorporated, meaning it is governed by the county but mostly manages its own affairs.
“We’re an hour and a half from the nearest emergency room, we don’t have acute care facilities on the island, and our ambulance system can be easily overwhelmed,” said Dr. John Osborn, who works as an emergency room physician in Seattle and also leads Vashon’s Medical Reserve Corps. “The challenges we face are faced by many other rural communities.”
After Dr. Bristow’s initial frustrations, he eventually got in touch with Dr. Osborn and the reserve corps. They came up with a plan for a coronavirus response team on the island. Another 70 volunteers joined the island’s corps to help — many of them older and at higher risk of dying or contracting severe disease if they are exposed. “We have a volunteer work force we simply can’t expose,” said Dr. Bristow, also the former deputy director of the Joint Genome Institute at Lawrence Berkeley National Laboratory in California.
Dr. Zach Miller, a resident of Vashon who set up the infectious disease department at the nonprofit regional health care system Group Health (now part of Kaiser), quickly realized that nasal swabs could be used in lieu of the clinically standard nasopharyngeal swabs, skirting the need for more extensive personal protective equipment such as face shields and N95 masks. “This can allow the model to be replicated in other places with a group of well-trained volunteers,” he said.
Since April 7, a historic building in the center of Vashon has been transformed into a coronavirus testing site. For a few hours every day, volunteers set up tents and tables outside and don medical masks and gloves to help residents get tested for coronavirus infection. Residents drive up and use their vehicles as personal waiting rooms. But instead of a trained medical practitioner inserting a swab deep into their nose, each patient gets a kit from a volunteer, stops their car and takes the swab themselves.
Image

So far, this testing setup has swabbed about 60 individuals, but not turned up any positive residents. (Vashon had four other coronavirus cases that were reported to the Washington Department of Health.) Dr. Bristow’s wife was never tested and has since recovered, and there hasn’t been a positive case on the island in over two weeks.
If the testing does turn up positive cases, some volunteers have been trained as contact tracers to identify people who have been in contact with the infected person.
“It’s not rocket science and with the right supervision you can train basically anyone to do it,” Dr. Bristow said. Moreover, having someone within the community trace call others might be advantageous because there is more inherent trust.
Image
The success of the Vashon method has relied on its medical reserve corps, a regional emergency preparedness team established by the federal government after the Sept. 11 attacks. Until coronavirus made its way to the West Coast, the corps on Vashon was most concerned with preparing for a massive earthquake expected to strike the Pacific Northwest. Dr. Osborn believes that the 829 Medical reserve corps around the country can be a building block for effective testing and tracing in other rural communities.
Currently, Dr. Bristow and Dr. Osborn are bringing their model to native nations in the Puget Sound and the Columbia River Basin, where Dr. Osborn had pre-existing relationships from his work on protecting rivers and salmon in the area. Like Vashon, many of these communities are relatively remote.
“We really welcomed this idea,” said Fawn Sharp, president of the Quinault Indian Nation in Taholah, Wash.
The reservation is about a 45-minute drive to the nearest emergency room, and has one ambulance for about 3,500 people.
“If coronavirus hits here, we are going to be hit hard, so we’re taking every precaution we can,” said M’Liss DeWald, the planning chief for Quinault’s coronavirus incident command team.
Ms. DeWald says that she and others in the community have many of the ingredients to implement the Vashon model — with eager volunteers and a physical location to do the testing. But early on they struggled with procuring test kits.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
Being able to implement the model would largely depend on the financial means to purchase test kits and certain protective gear, such as surgical masks and gloves, Dr. Henning-Smith said. Dr. Bristow suggests coronavirus response teams partner with clinics that have access to such gear. In the Lower Elwha Klallam Tribe on the Olympic Peninsula in Washington, medical workers have been able to repurpose many of their existing supplies to do testing for the coronavirus, said Dr. Brenda Powell, the tribe’s health services director.
Transportation might also be an issue in some rural communities. “How can you do a drive-through if people don’t have cars?” said Dr. Jasmeet Bains, describing one of the biggest challenges for the model. As a family medicine doctor in Taft, Calif., she primarily serves uninsured, undocumented immigrants who walk to her clinic.
Image
The Vashon model is very flexible, Dr. Miller said. Home test kits can be delivered to someone’s doorstep and picked up later, he said. The supply-chain bottlenecks that rural communities run into today might change tomorrow.
“If communities are going to test, they need to be able to adapt,” Dr. Bristow said. He plans on keeping the webpage for the Vashon model up-to-date, and hopes it “can be a clearinghouse for information in this rapidly changing landscape.”