A decade-long search for a treasure hidden deep in the Rocky Mountains that led to multiple people’s deaths is over, the man who hid the treasure announced.
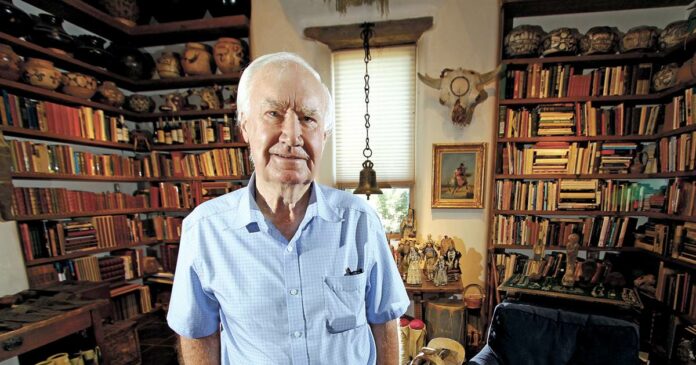
Forrest Fenn, a New Mexican art dealer, revealed on Sunday that his famed treasure was found, according to a post on his website that he confirmed to NBC News.
Let our news meet your inbox. The news and stories that matters, delivered weekday mornings.
The treasure, placed in a 13th-century Romanesque bronze chest, was hidden between 2009 and 2010 with an estimated $2 million of gold, jewelry and gems, the 89-year old said.
Tucked “somewhere in the mountains north of Santa Fe,” the bounty was either in New Mexico, Colorado, Wyoming or Montana, but Fenn did not specify in his announcement where exactly it was found.
“It was under a canopy of stars in the lush, forested vegetation of the Rocky Mountains and had not moved from the spot where I hid it more than 10 years ago,” Fenn wrote.
The art dealer left searchers nine clues in his memoir to help them find the treasure and said the hunt was meant to get people outside and explore nature. But the hints weren’t enough to keep many of them safe. In the decade between its hiding and discovery, multiple people died in their search.
In 2017, New Mexico urged people to stop looking for the treasure after someone died in the search. And one searcher died as recently as March.
“I congratulate the thousands of people who participated in the search and hope they will continue to be drawn by the promise of other discoveries,” Fenn wrote.