David Oliver, USA TODAY
Published 9:50 a.m. ET July 24, 2020
CLOSE![]()
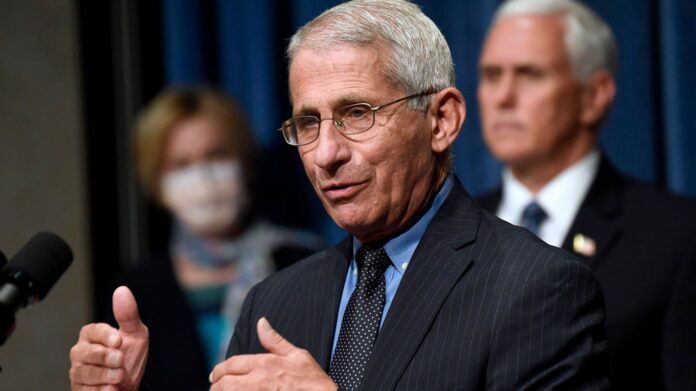
Dr. Anthony Fauci speaks to how personal responsibility and social distancing is the key to ending the spread of the coronavirus.
USA TODAY
You may be debating whether you want to get on a plane anytime soon. One person not debating is Dr. Anthony Fauci, who says he won’t be taking off during the coronavirus pandemic.
Fauci, the director of the National Institute of Allergy and Infectious Diseases at the National Institutes of Health, told MarketWatch that taking a flight is risky right now. And because he’s in an older age bracket, he’s not willing to take the risk.
“I am in a risk category,” Fauci said. “I don’t like to admit it, but I’m 79 years old. I can’t think of a reason to go trans-Atlantic. Right now, I’m very sequestered. I’m on a coronavirus task force. I go to the White House almost every day.”
Fauci said he spends half his day in his office working to develop a vaccine and drugs for COVID-19, which has now infected more than 4 million Americans.
“I don’t fancy seeing myself getting infected, which is a risk when you’re getting on a plane, particularly with the amount of infection that’s going on right now,” he said.
Is it safe to fly?: Here’s how to mitigate risk when flying during the coronavirus pandemic
Fauci also questioned the effectiveness of temperature checks before flights, something airlines have been pushing the U.S. federal government to start. “I’m not sure taking temperatures is all it’s cracked up to be because there are a lot of false negatives and false positives,” he said. “It’s best to just question people: ‘Do you have any symptoms? Have you been near someone who is infected?’ The time spent asking a couple of simple questions is probably more effective than just taking temperatures, to be honest with you.”
Uh oh: Airlines were finally starting to see passengers return. Then coronavirus cases spiked
5 flights in 4 weeks: What it’s really like to fly during the coronavirus pandemic
Should you fly amid COVID-19?
In spite of all the precautions now in place, Joseph Khabbaza, a pulmonary and critical care physician at the Cleveland Clinic, said flying offers the most potential of travel activities for exposure to the coronavirus, because of the nature of how planes are configured.
“Once you’re in the cabin, you don’t know who’s on the plane,” he said. “You’re in relative closer proximity to people you don’t know.”
Still, he said, flying is safer than it was earlier in the pandemic because of the changes airlines have made.
In addition to spacing and sanitizing, he said face masks add an extra layer of protection from the virus. Most U.S. carriers now require passengers to wear them.
Airlines, airports, the Transportation Security Administration and others have touted intensive new cleaning measures and safety protocols including mask requirements, social distancing, plexiglass partitions at ticket and gate counters and other precautions in a bid to protect employees and lure skittish vacation and business travelers back.
But cases have spiked, and based on recent earnings reports, airlines are still struggling.
United said Tuesday it will operate at barely over one-third of capacity through September as the coronavirus throttles air travel.
United CEO Scott Kirby said that demand has taken a step backward in July from where it was in mid-June, but it now seems to have bottomed.
“We expect we’re kind of back to where we were in late May and that demand will start to gradually recover once again as we get through the rest of the year,” he added.
Executives from Southwest, American, Spirit and Alaska airlines also detailed the sudden falloff in already shrunken travel demand in a series of quarterly earnings conference calls Thursday, echoing recent reports from United and Delta.
“In short, the crisis continues,” American CEO Doug Parker said. “This is less about people’s concern about flying and much more about having a reason to travel.”
Contributing: Curtis Tate and Dawn Gilbertson, USA TODAY; The Associated Press
‘More likely months than weeks’: Fauci warns UK coronavirus travel restrictions won’t lift anytime soon
Blast from the past: Why did US break Diamond Princess coronavirus quarantine? ‘Something went awry’
Autoplay
Show Thumbnails
Show Captions
Read or Share this story: https://www.usatoday.com/story/travel/news/2020/07/24/fauci-explains-why-he-wont-fly-amid-covid-19/5500501002/